Vascular & Vein Clinic
Varicose Vein & Spider Vein
What is it?
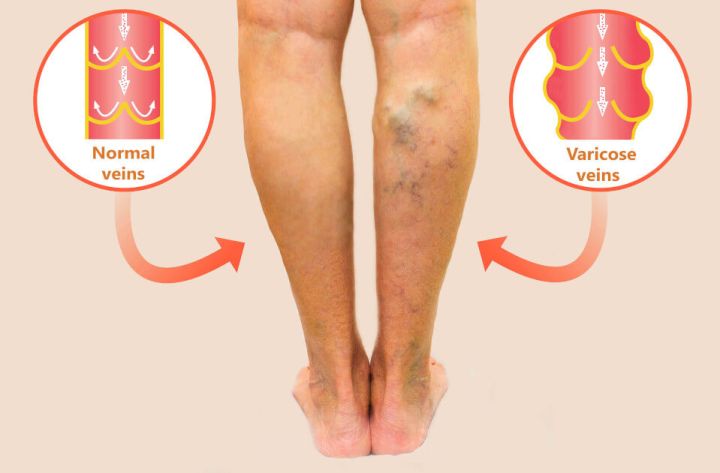
Varicose veins are enlarged, twisted, bluish veins that appear beneath the skin, most often on the legs. They result from poor circulation due to weakened vein walls or malfunctioning valves that allow blood to pool instead of flowing properly back to the heart. In addition to being visible, they can cause discomfort such as heaviness, aching, throbbing, swelling, warmth, itching, or leg cramps—especially after long periods of standing or sitting. Spider veins, by contrast, are smaller, more superficial, usually painless, and do not develop into varicose veins, although both may appear in the same area.
More than a cosmetic concern, varicose veins are often a sign of deeper venous dysfunction. If left untreated, they can lead to chronic venous insufficiency, which may progress to leg swelling (edema), skin changes, venous ulcers, or serious complications like blood clots, deep vein thrombosis (DVT), or pulmonary embolism. Early treatment is essential to relieve symptoms, prevent progression, and protect long-term vascular health.


Contributing factors include
What are the causes?
Aging and weakened vein walls
With age, the walls of the veins can become thinner and less able to maintain their structure. This gradual weakening reduces their ability to support healthy blood flow and affects how well the one-way valves function. When the valves no longer close properly, blood starts to flow backward and pool in the legs, increasing pressure inside the veins. Over time, this buildup of pressure stretches the vein walls, making them bulge and twist, which contributes to the visible appearance of varicose veins.
Poor leg muscle tone
The leg muscles, particularly the calf muscles, play a crucial role in moving blood back up toward the heart. This natural mechanism, known as the calf muscle pump, relies on regular muscle contractions to support healthy blood flow and reduce pressure in the lower limbs. When the leg muscles are underused—due to lack of physical activity, prolonged sitting, or sedentary habits—the pump loses efficiency. This can lead to increased venous pressure, contributing to the dilation of veins and the progression of venous insufficiency or varicose veins. Over time, symptoms like leg swelling, heaviness, and swollen veins may become more pronounced.
Prolonged positions
Prolonged standing or sitting disrupts normal blood flow in the lower limbs, leading to venous stasis—a condition where blood pools in the veins instead of circulating efficiently. When combined with reduced calf muscle activity or general inactivity, this stagnation increases pressure on the vein walls. Over time, this can contribute to the development of superficial varicose veins, as well as more serious complications like deep vein thrombosis (DVT). These changes may result in symptoms such as swollen veins, leg swelling, and visibly twisted veins in the affected areas.
Pregnancy
During pregnancy, the growing uterus puts increasing pressure on the pelvic and leg veins, which can significantly restrict venous return and cause blood to pool in the lower limbs. This added pressure, along with hormonal changes, can weaken the vein walls and reduce the effectiveness of the one-way valves that normally keep blood flowing upward. As a result, many women develop new varicose veins, especially on the legs and ankles. The likelihood of experiencing swollen veins, venous insufficiency, leg swelling, and a persistent feeling of heaviness is also higher during pregnancy.


How to prevent?
Regular physical activity—such as walking, cycling, or swimming—keeps the calf muscles engaged and helps stimulate healthy blood flow through the leg veins. This muscle action supports the return of blood to the heart and prevents it from pooling in the lower limbs, which is essential to reduce pressure inside the veins and protect their long-term function.
A diet rich in fiber and low in salt helps reduce water retention and leg swelling, while supporting healthy circulation. Limiting sodium also helps regulate blood pressure, easing the strain on vein walls. Antioxidant-rich foods like berries, citrus fruits, and leafy greens contribute to maintaining strong, healthy veins and minimizing the risk of vein-related complications.
Excess weight puts additional pressure on the lower body, especially the leg veins, as they must work harder against gravity to return blood to the heart. This increased pressure can strain the one-way valves responsible for keeping blood moving upward. Over time, the extra load may weaken the vein walls, disrupt normal circulation, and lead to the development or worsening of varicose veins. Maintaining a healthy weight through balanced nutrition and regular activity helps relieve this pressure and supports long-term vascular health.
Avoid prolonged periods of sitting or standing, as these can slow blood circulation and cause blood to accumulate in the lower limbs. Moving regularly throughout the day and elevating your legs when possible helps relieve vein pressure, improve flow, and prevent the onset or worsening of symptoms like swelling or heaviness.
Tight clothing, especially around the legs or waist, can restrict circulation and place unnecessary pressure on the veins. Choosing looser garments helps preserve normal blood flow. High heels should also be avoided, as they reduce calf muscle activation and limit the upward movement of blood toward the heart.
Hot baths, saunas, and prolonged exposure to high temperatures can cause the veins to dilate, increasing vein pressure and worsening varicose vein symptoms such as swelling or heaviness. Opting for lukewarm showers helps protect blood circulation and reduces unnecessary stress on the veins.
Compression stockings apply gentle, graduated pressure to the legs, supporting blood flow, reducing swelling, and helping prevent the formation of new varicose veins. This form of compression therapy is particularly helpful after treatment or for individuals with a personal or family history of vein problems. It also plays a role in reducing the risk of complications such as deep vein thrombosis (DVT) and can improve daily comfort for those experiencing chronic symptoms.
How to Treat
Endovenous laser (EVL or EVLT)
Endovenous laser treatment (EVL or EVLT) is a minimally invasive procedure used to treat varicose veins caused by deeper, non-functioning veins. Recognized as a gold standard and widely used in Canada since 2002, it offers an effective alternative to traditional surgical vein stripping. The treatment involves inserting a fine laser fiber into the affected vein under local anesthesia. A protective solution is injected around the vein, and once the laser is activated, it delivers intense heat—exceeding 800°C—to seal the vein from the inside, stopping reflux and restoring healthy blood flow.


Ultrasound-Guided Sclerotherapy (Foam Sclerotherapy)
Foam sclerotherapy is a minimally invasive treatment used to target larger varicose veins that lie deeper beneath the skin and are not always visible. Guided by ultrasound, a healthcare provider injects a sclerosing solution that has been mixed with air to create a foam. This foam spreads evenly along the vein walls, promoting an effective closure. As the treated vein collapses and is gradually reabsorbed by the body, blood flow is redirected to healthier veins, helping relieve symptoms like heaviness, swelling, and fatigue in the legs.
Sclerotherapy
Sclerotherapy is a minimally invasive treatment used to target visible varicose veins and spider veins near the surface of the skin. A healthcare provider injects a special solution, called a sclerosing agent, directly into the affected vein. This substance irritates the inner lining of the vein, triggering a process called fibrosis, which causes the vein to collapse and eventually be reabsorbed by the body. As the blood is redirected to healthier veins, the treated vein fades from view over time.